Millimeters and Meaning: Why Surgical Finesse Matters
Inside the High-Stakes World of Millimeter-Scale Decision-Making
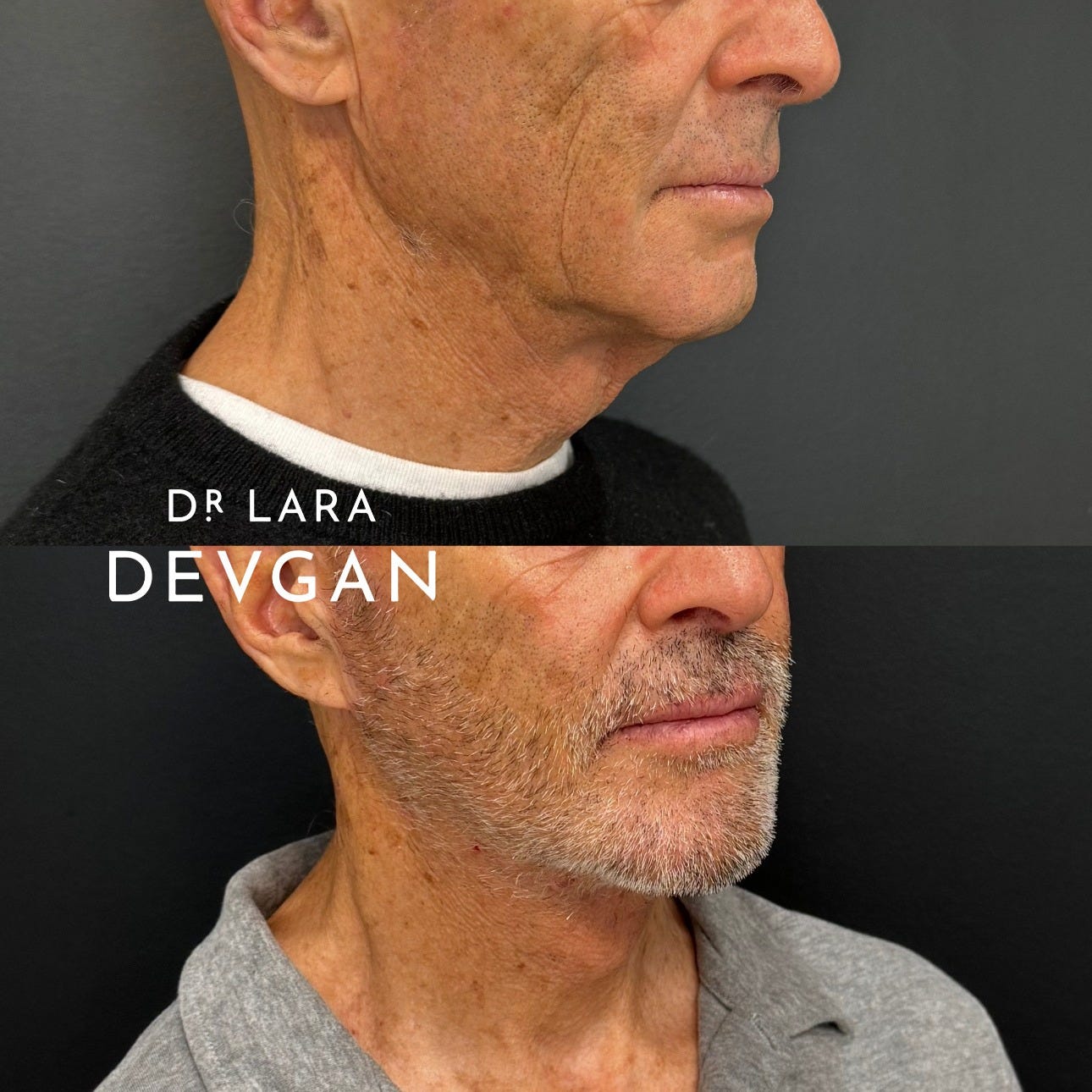
In aesthetic plastic surgery, the smallest shifts yield the most significant results. We do not work in inches—we work in millimeters. And when performed with precise anatomical understanding, millimeter-scale changes to the face can create dramatic improvements in facial balance, youthful structure, and emotional expressiveness.
This is especially true in procedures that define the framework of the face: midface lift, lower facelift, necklift, temporal brow lift, upper and lower blepharoplasty, lip lift, buccal fat pad excision, chin implant, rhinoplasty, autologous fat grafting, and erbium laser resurfacing.
Today’s patients do not want to look “done.” They want to look more like themselves—rested, alert, elegant, and confident. This requires surgical finesse: the marriage of anatomical fluency, restraint, and technical control.
I. The Surgical Impact of One Millimeter
Studies confirm that facial perception is highly sensitive to micro-changes in structure. In a landmark study published in Plastic and Reconstructive Surgery, Horlock et al. found that a 2 mm asymmetry in facial contour is consistently perceived by laypeople and surgeons alike—and affects ratings of attractiveness, trustworthiness, and age perception.1
This matters profoundly in facelift surgery. In the midface, millimeters of vertical elevation at the deep malar fat pad can restore youthful anterior projection, but excess vector tension or lateral displacement will create an unnatural sweep. In lower facelifts, excessive skin pull—sometimes just 1–2 mm too far—can distort the angle of the mandible or ear tragus, betraying the surgical outcome.
Similarly, in necklifts, anterior platysmal approximation must be precisely midline and tension-balanced. According to Rohrich et al., overcorrection or undercorrection of even 3–5 mm in the cervicomental angle can compromise both aesthetic and functional results.2
When analyzing preoperative photographs or planning incisions, surgeons must consider not only soft tissue redundancy but also deep structural shifts. Advanced 3D imaging, cephalometric measurements, and calibrated skin tension tests have improved surgical predictability, but real-time intraoperative judgment remains irreplaceable.
Keep reading with a 7-day free trial
Subscribe to Plastic by Dr. Lara Devgan to keep reading this post and get 7 days of free access to the full post archives.